Associated with labral tears
May extend between scapular spine and glenoid cavity
May be seen in suprascapular notch, where it may result in neural compression, leading to muscle atrophy
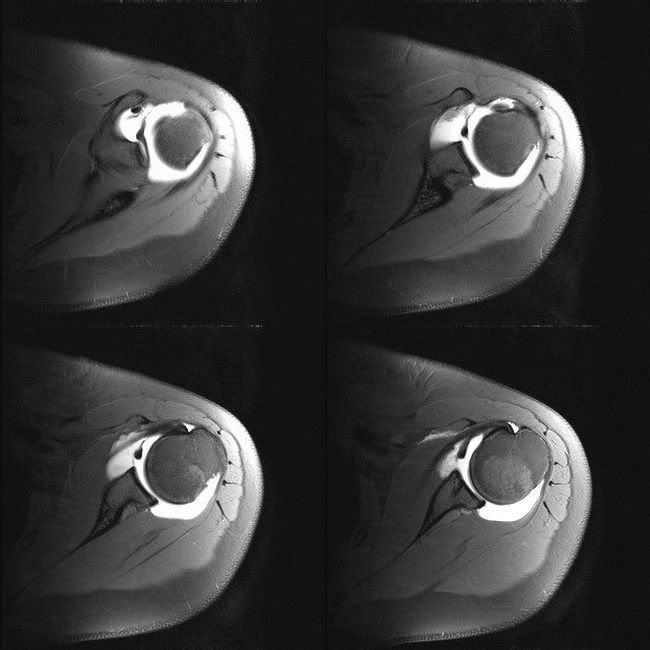
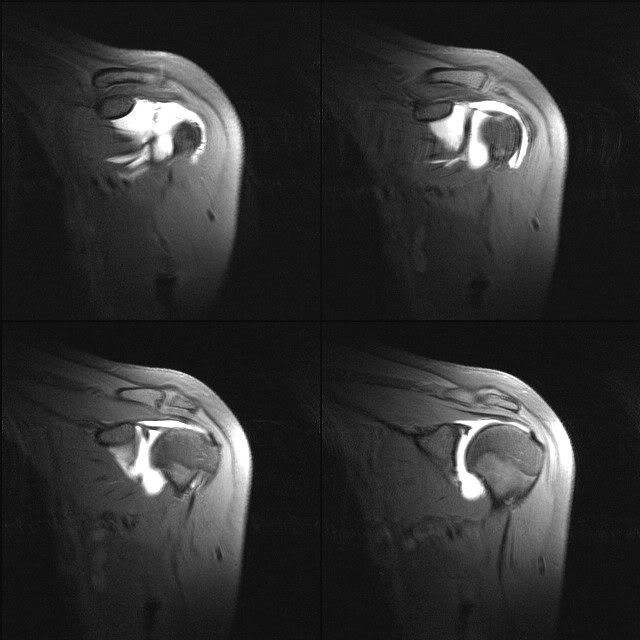
PSGI
Posterosuperior glenoid impingement
Partial thickness tear of the infraspinatus at the junction of supraspinatus
Posteosuperior labral tear
Posterosuperior humeral head microfractures
Partial thickness tear of the infraspinatus at the junction of supraspinatus
Posteosuperior labral tear
Posterosuperior humeral head microfractures
Capsule of glenohumeral joint
Anterior capsule attachment:
Type I: insertion at glenoid margin
Type II: insertion at glenoid neck within 1 cm of labral base
Type III: insertion on the scapula more than 1 cm from the labral basze
The further the capsule attaches, the more unstable the joint
Overdistended MR arthrography may produce type III insertion
Type I: insertion at glenoid margin
Type II: insertion at glenoid neck within 1 cm of labral base
Type III: insertion on the scapula more than 1 cm from the labral basze
The further the capsule attaches, the more unstable the joint
Overdistended MR arthrography may produce type III insertion
Buford complex
Sublabral recess
Normal synovial reflection between glenoid cartilage and superior labrum
Seen at 12 O clock position at the attachment of biceps
May be continuous with sublabral foramen
May be misinterpreted as SLAP II injury
Seen at 12 O clock position at the attachment of biceps
May be continuous with sublabral foramen
May be misinterpreted as SLAP II injury
Sublabral foramen
Normal localised detachment of the anterosuperior labrum from the glenoid
Seen at 2 O clock position, anterior to the biceps attachment
Difficult to distinguish from SLAP injury
No residual labral tissue on the glenoid
Anterosuperior labrum is not attached to the glenoid rim
Labrum has a smooth margin and reattaches at 3 O clock position
Also note that isolated SLAP injury is rare, but can occur in throwing athletes
Seen at 2 O clock position, anterior to the biceps attachment
Difficult to distinguish from SLAP injury
No residual labral tissue on the glenoid
Anterosuperior labrum is not attached to the glenoid rim
Labrum has a smooth margin and reattaches at 3 O clock position
Also note that isolated SLAP injury is rare, but can occur in throwing athletes
Overview of MR arthrography of shoulder
Contrast:
0.1-0.2 mL of Gd in 20 mL of saline
12-20 mL
Sequences:
T1 FS - axial, coronal, sagittal, ABER
T2 FSE/ STIR - coronal
Axial:
SGHL - parellal to corocoid process
MGHL - parellal to subscapularis
IGHL - seen in axillary recess
Coronal:
Long head of biceps
MGHL
Superior labrum - seen as a triangle
Sagittal:
Anterior band of IGHL - seen from 3 O clock position
Coracohumeral ligament
ABER view:
Anterior band of IGHL is continouous with anteroinferior labrum
Pathologies:
Most of the normal variants occur between 11 and 3 O clock postion
Most of the pathologies occur between 3 and 6 O clock position
0.1-0.2 mL of Gd in 20 mL of saline
12-20 mL
Sequences:
T1 FS - axial, coronal, sagittal, ABER
T2 FSE/ STIR - coronal
Axial:
SGHL - parellal to corocoid process
MGHL - parellal to subscapularis
IGHL - seen in axillary recess
Coronal:
Long head of biceps
MGHL
Superior labrum - seen as a triangle
Sagittal:
Anterior band of IGHL - seen from 3 O clock position
Coracohumeral ligament
ABER view:
Anterior band of IGHL is continouous with anteroinferior labrum
Pathologies:
Most of the normal variants occur between 11 and 3 O clock postion
Most of the pathologies occur between 3 and 6 O clock position
Ultrasound
Differentiating effusion from synovitis:
1. Effusion is compressible, synovitis is not
2. Switch on Doppler, synovitis may light up, effusion will not
1. Effusion is compressible, synovitis is not
2. Switch on Doppler, synovitis may light up, effusion will not
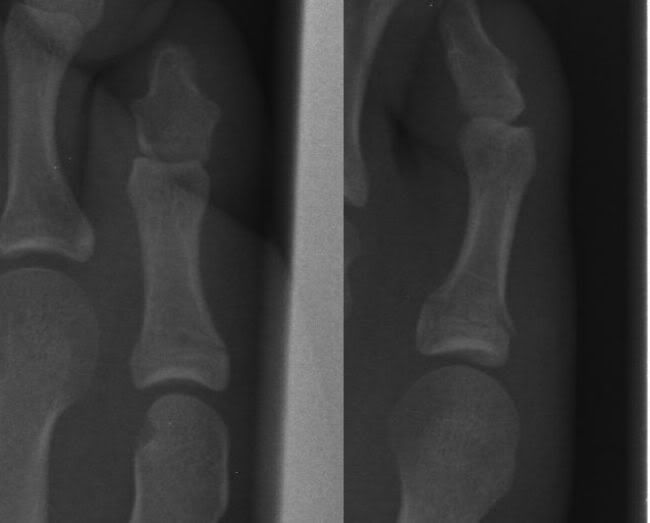
Lisfranc fracture dislocation
Plain radiographs:
AP view:
Alignment of lateral border of 1st metatarsal base with lateral border of medial cuneiform
Alignment of medial border of 2nd metatarsal base with medial border of middle cuneiform
First intermetatarsal gap should be less than 2 mm
Fleck sign in 1st intermetatarsal gap (flake fracture)
Oblique view:
Alignment of medial and lateral borders of 3rd metatarsal with lateral cuneiform
Alignment of medial border of 4th metatarsal with medial border of cuboid
Lateral view:
Step-off sign: dorsal displacement of 2nd metatarsal base compared to tarsal bones
References:
Injury Extra, Volume 38 (2007), 250-254
Image gallery:

AP view:
Alignment of lateral border of 1st metatarsal base with lateral border of medial cuneiform
Alignment of medial border of 2nd metatarsal base with medial border of middle cuneiform
First intermetatarsal gap should be less than 2 mm
Fleck sign in 1st intermetatarsal gap (flake fracture)
Oblique view:
Alignment of medial and lateral borders of 3rd metatarsal with lateral cuneiform
Alignment of medial border of 4th metatarsal with medial border of cuboid
Lateral view:
Step-off sign: dorsal displacement of 2nd metatarsal base compared to tarsal bones
References:
Injury Extra, Volume 38 (2007), 250-254
Image gallery:

Foot views
Image 1:

Findings: Lisfranc's dislocation of the left foot
Lesson: The line drawn along the medial border of the 2nd metatarsal should be aligned with the medial border of the middle cuneiform bone on the AP view.
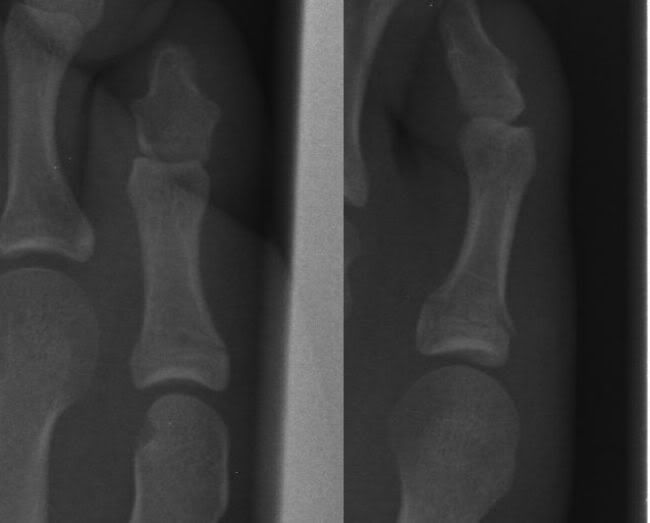
Image 2:

Findings: AVN of head of the 2nd metatarsal
Lesson: Not all rapid reporting films are post traumatic
Image 3:

Finding: fracture of PP of 3rd toe
Zoomed image:

Lesson: Phalanges fractures are common in rapid reporting
Image 4:

Findings: Fracture PP of little toe
Zoomed image:
Lesson: Phalanges fractures are common in rapid reporting

Findings: Lisfranc's dislocation of the left foot
Lesson: The line drawn along the medial border of the 2nd metatarsal should be aligned with the medial border of the middle cuneiform bone on the AP view.
Image 2:

Findings: AVN of head of the 2nd metatarsal
Lesson: Not all rapid reporting films are post traumatic
Image 3:

Finding: fracture of PP of 3rd toe
Zoomed image:

Lesson: Phalanges fractures are common in rapid reporting
Image 4:

Findings: Fracture PP of little toe
Zoomed image:
Lesson: Phalanges fractures are common in rapid reporting
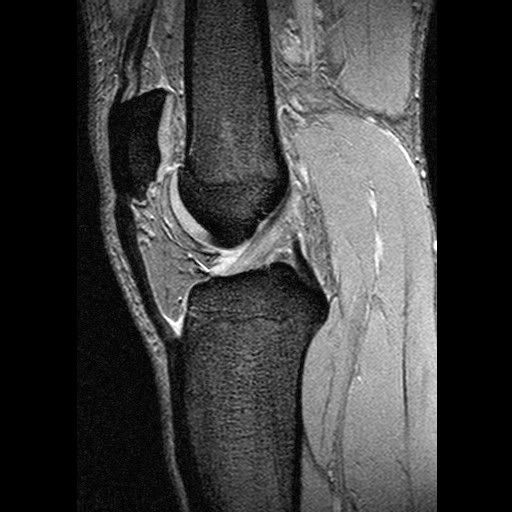
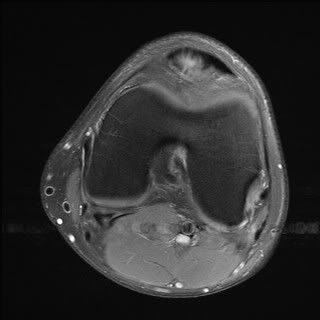
Discoid meniscus
Broad disc like configuration with loss of normal bow-tie
Considered congenital and frequently bilateral Thickness 5-13 mm (usually more than 13mm)
Incidence:
More common in LM. LM 1.5-15%, in MM 0.3%
Variant:
Anterior megahorn discoid meniscus
Pathology:
Susceptible to tears and cysts
Clinical features:
Most commonly present in adolescence, but most are asymptomatic
Complaints: pain, slipping, snapping, locking
Classification (Watanabe):
Complete: extends into intercondylar notch
Incomplete: does not extends into intercondylar notch. Most common
Wrisberg-ligament type: lacks posterior capsular attachment (posterior meniscotibial ligament) and occurs only in LM.
Plain radiograph:
Wide lateral joint space
Hypoplastic and squared-off lateral femoral condyle
High fibular head
Cupping of lateral tibial plateau
MR:
Sagittal (4-5mm thick slices):
Bow-tie in 3 or more images
No central tapering
Increased height
Coronal:
Increased height, more than 2 mm higher than the opposite meniscus
Extension into intercondylar notch
Radial diameter more than 13 mm
Considered congenital and frequently bilateral Thickness 5-13 mm (usually more than 13mm)
Incidence:
More common in LM. LM 1.5-15%, in MM 0.3%
Variant:
Anterior megahorn discoid meniscus
Pathology:
Susceptible to tears and cysts
Clinical features:
Most commonly present in adolescence, but most are asymptomatic
Complaints: pain, slipping, snapping, locking
Classification (Watanabe):
Complete: extends into intercondylar notch
Incomplete: does not extends into intercondylar notch. Most common
Wrisberg-ligament type: lacks posterior capsular attachment (posterior meniscotibial ligament) and occurs only in LM.
Plain radiograph:
Wide lateral joint space
Hypoplastic and squared-off lateral femoral condyle
High fibular head
Cupping of lateral tibial plateau
MR:
Sagittal (4-5mm thick slices):
Bow-tie in 3 or more images
No central tapering
Increased height
Coronal:
Increased height, more than 2 mm higher than the opposite meniscus
Extension into intercondylar notch
Radial diameter more than 13 mm
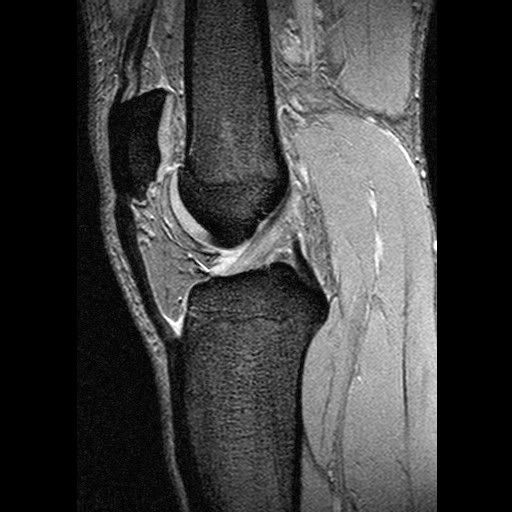
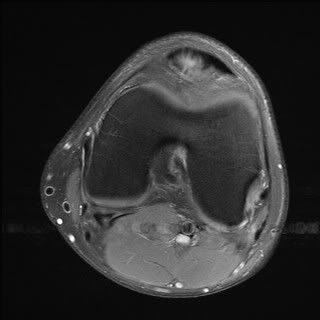
Patellar tendinosis
Patellar tendinosis: (Jumper's knee)
Acute less than 2 weeks
Chronic more than 2 weeks
Mechanism:
Common in basketball and volleyball players
Due to malialignment
Common in adults
Pathology:
Patellar insertion (proximal tendon) more often than tibial insertion
Posterior surface more prone than superficial
Medial side more common than lateral side
USG:
Disruption of normal fibrillary pattern, swelling, hypoechoes, calcium, hypervascularity
Paratenonitis seen as thickening with echopoor area peripherally
MRI:
Best seen on sag and axials
Intermediate signal on T1, high on T2 and STIR, may enhance on Gd
Edema in the inferior patella
Focal thickening (convex posterior margin)
Poorly defined posterior margin
Management:
Conservative.
Surgery, if failed conservative treatment, cystic or mucoid degreneration, osteophytosis.
USG guided autologous blood injection, sclerosant injection can be used to treat hypervascular tendinopathies.
USG guided steroid, if marked Hoffitis.
References:
1. Peace KAL et al. Imaging the infrapatellar tendon in the elite athlete. Clin Rad (2006) 61, 570-578
2. Stoller DW. MRI in orthopaedics & sports medicine; Second edition; 1997. Chapter 7: the knee. Lippincott Williams & Wilkins.
Journal watch: Click Here
Image Gallery:
Thick patellar tendon:
Significantly thickened patellar tendon:

Signal change in the inferior pole of patella:

Associated Hoffa's fat inflmmation:

Convexity and high signal in the medial aspect of the posterior part of the patellar tendon:
Acute less than 2 weeks
Chronic more than 2 weeks
Mechanism:
Common in basketball and volleyball players
Due to malialignment
Common in adults
Pathology:
Patellar insertion (proximal tendon) more often than tibial insertion
Posterior surface more prone than superficial
Medial side more common than lateral side
USG:
Disruption of normal fibrillary pattern, swelling, hypoechoes, calcium, hypervascularity
Paratenonitis seen as thickening with echopoor area peripherally
MRI:
Best seen on sag and axials
Intermediate signal on T1, high on T2 and STIR, may enhance on Gd
Edema in the inferior patella
Focal thickening (convex posterior margin)
Poorly defined posterior margin
Management:
Conservative.
Surgery, if failed conservative treatment, cystic or mucoid degreneration, osteophytosis.
USG guided autologous blood injection, sclerosant injection can be used to treat hypervascular tendinopathies.
USG guided steroid, if marked Hoffitis.
References:
1. Peace KAL et al. Imaging the infrapatellar tendon in the elite athlete. Clin Rad (2006) 61, 570-578
2. Stoller DW. MRI in orthopaedics & sports medicine; Second edition; 1997. Chapter 7: the knee. Lippincott Williams & Wilkins.
Journal watch: Click Here
Image Gallery:
Thick patellar tendon:
Significantly thickened patellar tendon:

Signal change in the inferior pole of patella:

Associated Hoffa's fat inflmmation:

Convexity and high signal in the medial aspect of the posterior part of the patellar tendon:
Subscribe to:
Posts (Atom)