Not surrounded by synovial sheath
Surrounded by loose connective tissue - peritenon
MR:
Uniformly low signal
Flattened or slightly concave anterior border
Less than 1 cm in AP thickness
TENDINOPATHY:
Diffuse or focal
Acute or chronic
Mechanical (proximal medially) or inflammatory (distal, associated with spondyloarthropathies)
Ultrasound:
Increase in the thickness, becomes more rounded (normally anterior margin is flat or concave)
Decrease in overall echogenicity, often on posterior aspect
Associated paratenon thickening (paratenonopathy)
Neovascularization may be seen, often in anterior aspect
Insertional tendinitis:
Repetitive microtrauma
Common in ballet dancers, runners, jumpers; also in RA and seronegative arthropathies
MR:
Thick tendon at insertion
Loss of normal anterior concavity
Intrasubstance abnormal signal
Treatment:
Numerous, USG guided procedures include steroid injection, dry needling, autologous blood injection
TEAR (RUPTURE):
Common in 40-50 years
Risk factors: hyperlipidaemia
Most common site: mid tendon, 5-6 cm above the insertion; associated with tendinopathy; 30-50 years; often acute
Other sites: MTJ (should be differentiated fomr aponeurotic shear tear (entire belly of medial gastrocnemius) and avulsion from insertion (associated with avulsion fracture)
Plain radiograph:
Soft-tissue density in Kager's fat pad
Thickening of the tendon
Positive Arner's sign - tendo achillis deviates anteriorly, thus nonparalleling the skin surface
Decreased Toygar's angle - angle of the posterior skin surface adjacent to the tendo achillis; less than 150° is indicative of tendoachillis rupture
Ultrasound:
Full thickness interruption, filled with fluid, blood, debris
Dynamic gentle dorsi and plantar flexion is helpful
If the gap is more than 5 mm in plantar flexion, surgery is indicated
The gaps less than 5 mm are managed conservatively
XANTHOMA OF ACHILLIS:
Ultrasound:
Focal hypoechoic lesions
MR:
Axials: Diffuse speckled or reticulated pattern on all sequences, more obvious on fat-sat T1
Probably due to edema or inflammation, not intratendinous lipid
Retrocalcaneal bursitis
Haglund's syndrome
References:
1. Ly JQ et al. Anatomy of and Abnormalities Associated with Kager's Fat Pad . AJR 2004; 182:147-154
2. McNally EG. Practical musculoskeletal ultrasound. Churchill Livingstone 2005
Journal watch: Click Here
Ultrasound Image Gallary:
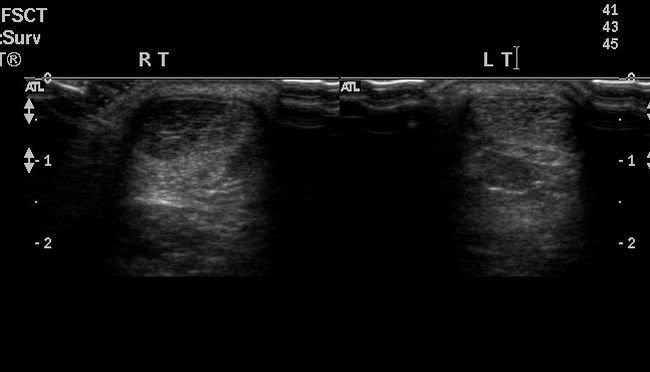
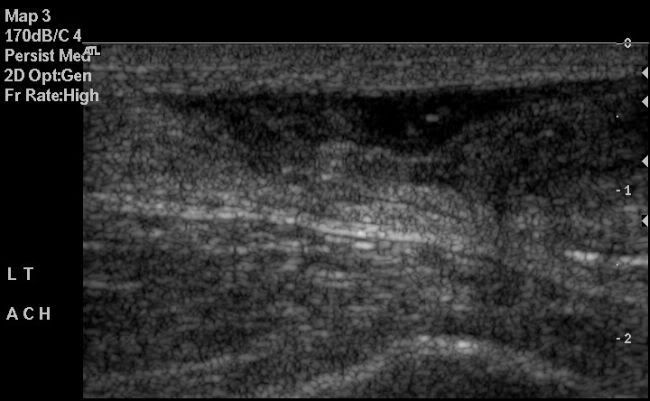
Achillis tendiopathhy: Compare with the normal side
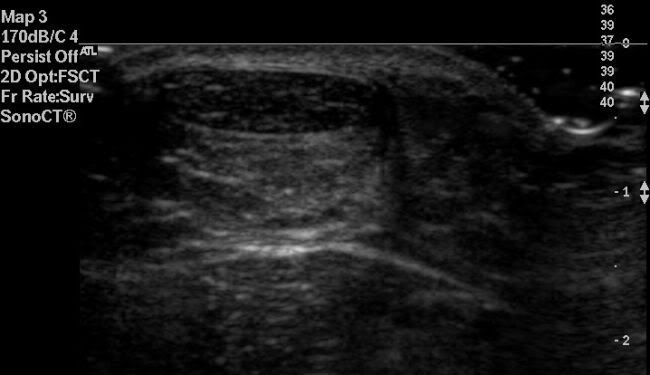
Achillis tendinopathy ultrasound long axis:

Achillis tendinopathy ultrasound short axis:
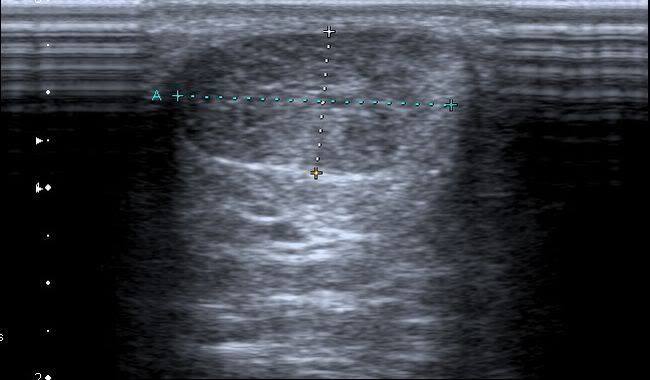
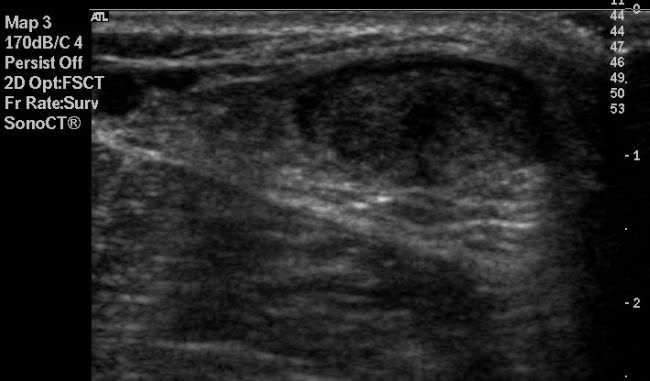
Achillis MTJ rupture:
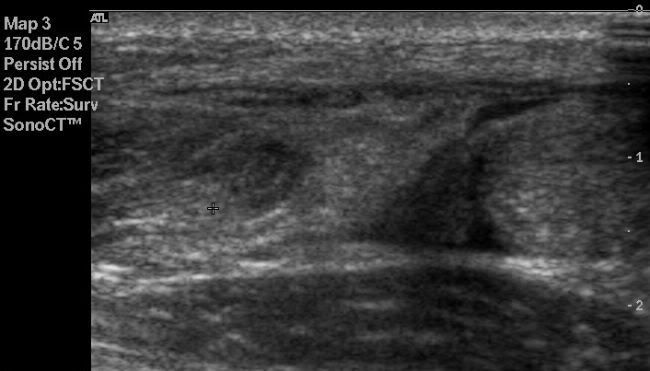
Mid Achillis tendon rupture long axis:
Mid Achillis tendon rupture short axis:
Grade I muscle injury in gastrocnemius: